Hypothalamic Obesity (HyOb)
What Is Hypothalamic Obesity?
Hypothalamic Obesity (HyOb) is a rare and complex condition resulting from damage or dysfunction of the hypothalamus, often due to tumors (such as craniopharyngiomas), surgery, trauma, or genetic disorders. The hypothalamus plays a crucial role in regulating appetite, metabolism, and energy balance.
In HyOb, impaired signaling leads to uncontrollable weight gain, reduced energy expenditure, and resistance to conventional weight-loss strategies. Management typically includes lifestyle interventions, medications, and, in some cases, bariatric or neuromodulatory therapies.
Despite being tiny, the hypothalamus, which is found near the base of the brain, controls a wide range of vital physiological processes, including hormone release, appetite control, fluid balance, body temperature, sleep cycles, and the maintenance of the body’s internal energy balance (metabolic rate).
There are at least two main ways that abnormal hypothalamus function contributes to obesity: In addition to having a slow metabolism, which results in less energy being produced and a lower calorie expenditure, a child may have hyperphagia, an excessive demand for food. When these two things happen at the same time, weight gain may start quickly. Disruption of hormone synthesis, sleep, and circadian rhythms are just a few of the ways that abnormal hypothalamus function can impact energy balance. These disruptions may result in weariness and a decrease in physical activity.
The hypothalamus’ potential role in social functioning, which may influence eating and activity habits, is another area of recent study.
Hypothalamic obesity is the result of an imbalance between a person’s energy intake from food and the amount of energy their body has expended due to damage to the hypothalamus.
One little area of the brain that aids in a number of body processes is the hypothalamus. The management of energy intake and use is one crucial function. The term “use” describes the energy that the body requires for internal processes and activity, whereas “intake” describes the quantity of calories that a person consumes via food and drink.
Rapid weight gain that can be challenging to control may result from an imbalance between energy intake and use caused by hypothalamic injury. Hypothalamic obesity can cause a person to feel the desire to eat more or to have improper energy utilization.
The Distinction Between Hypothalamic Obesity and General Obesity
A rare form of obesity known as “hypothalamic obesity” is linked to damage to the brain’s amygdala or hypothalamus.When it is damaged, the person overeats because they are really hungry. Additionally, energy expenditure declines, leading to obesity.
This kind of obesity is not the same as general obesity, which is typically caused by consuming too many calories in comparison to the calories expended during physical activity.
Let’s go over the relevant body systems and anatomy: Located directly above the pituitary gland at the base of the brain is the hypothalamus. As a component of the endocrine system, it works in tandem with the pituitary gland to release and control hormones that are involved in numerous body processes, including:
- Hunger and thirst
- body temperature
- Food conversion to energy, or metabolism
- The beginning of puberty
- Sleep patterns
- gaining weight
When the hypothalamus is damaged, the usual hormonal balance is upset. A number of hormones interact to regulate metabolism, which is the breakdown of food into energy, and impact weight growth. These hormones include:
- The hormone that releases corticotropin (CRH), which affects metabolism
- GHRH (growth hormone-releasing hormone), which supports a balanced body composition
- Regulating appetite, sleep patterns, and body temperature is oxytocin.
- TRH is a hormone that helps regulate metabolism, energy, growth, and development.
Does Hypothalamic Obesity Occur Often? What’s the Cause?
Although it is uncommon in the general population, hypothalamic obesity is quite prevalent in those who have had a hypothalamic injury. Injuries to the hypothalamus are frequently caused by the excision of a craniopharyngioma, a noncancerous brain tumor. Children are frequently afflicted with these malignancies. Craniopharyngiomas are incredibly uncommon; approximately 0.5 to 2.5 new instances are diagnosed for every million persons annually.
Complete removal of the tumor with minimal harm to adjacent structures is the aim of medical professionals. Surgery that enters the base of the brain by the nose is frequently used to achieve this. Radiation therapy may potentially be used to treat the tumor.
The brain damage caused by craniopharyngioma treatment puts patients at risk for hypothalamic obesity even after a successful operation. This is why continuous observation is crucial.
Although there are additional reasons of hypothalamic obesity, brain tumors are the primary cause in many cases. The cycle might start if the hypothalamus is damaged. The hypothalamus may sustain injury from infection, inflammation, head trauma, or cerebral hemorrhage. Prader-Willi syndrome and Bardet-Biedl syndrome are two hereditary disorders linked to hypothalamic obesity.
What Function Does the Hypothalamus Serve in Controlling Appetite?
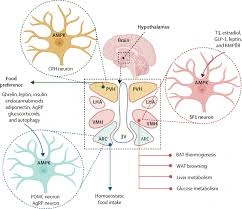
A key part of the brain, the hypothalamus is responsible for controlling appetite, weight, and metabolism. Hormones that regulate appetite, satiety, and metabolism, including proopiomelanocortin, ghrelin, leptin, and neuropeptide Y, are produced and released by neurons in this area. In order to help control appetite and energy expenditure, it sends out hormonal signals after receiving information from the intestines, liver, and adipose tissue, among other bodily organs.
Leptin: The hypothalamus receives this hormone, which is generated by adipose (fat) cells, as a signal that the body’s energy reserves are enough. It aids in appetite suppression and energy expenditure, which helps control body weight.
Ghrelin: On the other hand, when the body is feeling low on energy, the stomach produces a hormone called ghrelin, which interacts with the hypothalamus. It increases body weight by boosting appetite and lowering energy expenditure.
Neuropeptide Y: This hormone, which increases appetite, is generated by the hypothalamus. It is released in reaction to low blood levels of fatty acids or glucose, which signal a need for energy intake.
Proopiomelanocortin (PMOC): POMC inhibits appetite and promotes energy expenditure as part of its involvement in appetite regulation. By producing alpha-melanocyte-stimulating hormone (alpha-MSH), which operates on the brain to increase energy expenditure and decrease food intake, it accomplishes this.
Apart from controlling appetite, the hypothalamus also has an impact on metabolism. Thyroid-stimulating hormone (TSH), growth hormone-releasing hormone (GHRH), and corticotropin-releasing hormone (CRH) are among the hormones that it regulates in order to impact metabolism. The breakdown of nutrients and the transformation of food into energy are two aspects of the body’s energy consumption that these hormones aid in controlling.
Abnormal eating habits can result from damage to the hypothalamus, which can upset the delicate balance of these hormones. In addition, this disease can lead to additional health issues like insulin resistance, diabetes, and high blood pressure, as well as excessive weight gain and trouble decreasing weight.
Symptoms
One of the many bodily processes that the hypothalamus regulates is energy. Consequently, it may have varying effects on individuals.
People who have hypothalamic obesity may feel the need to eat all the time. This could occur in conjunction with the sensation of never being fully satisfied after eating.
Others gain weight even when they consume a healthy diet, exercise frequently, and limit their caloric intake. This is due to a decrease in the body’s resting metabolism. If someone leads a largely sedentary lifestyle, the impacts could get worse.
In these situations, a person may quickly put on weight that is hard to reduce using conventional weight-loss methods.
Some individuals who have hypothalamic obesity may also have hypopituitarism, a condition in which the pituitary gland produces insufficient amounts of certain hormones.
Endocrine hormone deficits may result from poor communication between the pituitary and hypothalamus in individuals who have injury to either gland. Some endocrine hormone abnormalities, such growth hormone insufficiency or hypothyroidism, can cause weight gain and obesity if left untreated.
A malfunctioning hypothalamus can also cause the following symptoms in a person:
- Problems with electrolyte and fluid balance
- complicated psychosocial repercussions, which describe the mental and social impacts of the illness
- difficulties controlling blood pressure and heart rate
- eyesight problems
- trouble controlling body temperature
- Sleep problems
- problems with the circadian rhythm
Causes
The degree of hypothalamic damage is directly correlated with the appearance of obesity, according to imaging studies, according to a 2022 study.
The primary cause of hypothalamic obesity is damage to the parts of the hypothalamus involved in energy management. Brain tumors or head injuries may be the cause of this. High brain pressure, a risk factor for future obesity, is indicated by swelling of the optic nerve at the time of initial diagnosis in patients with brain tumors.
Additionally, experts believe both genetic and environmental factors may influence the degree of childhood obesity and the likelihood of future childhood obesity. Apart from becoming obese during treatment, the following other factors may raise the chance of being obese in the future:
- reduced consumption of energy during both active and resting states
- A greater desire to eat
- reduced perception of fullness following meals
- persistently elevated blood levels of the hormone insulin, which aids in blood sugar regulation
- possible inability to use the hormone leptin, which aids in controlling appetite
- irregular sleep patterns and circadian rhythms
- Deficits in pituitary hormones
- Mental health issues that could have a detrimental impact on healthy habits like eating a balanced diet or exercising
In a 2019 study, scientists found the following potential reasons for hypothalamus damage:
- brain cancers, like craniopharyngiomas
- Radiation treatment with cranial irradiation
- circumstances related to genes
- inflammation.
- traumatic brain injury
They added that following hypothalamic damage, the following potential risk factors may be linked to the development of hypothalamic obesity:
- significant harm to the hypothalamus
- Endocrine dysfunction present at the time of diagnosis
- age of diagnosis—the researchers hypothesize that younger kids are more likely to be obese.
- being more substantial when diagnosed
- obesity in the family
- excessive radiation exposure to the hypothalamus region
Which hypothalamic obesity consequences exist?
The condition’s complications include:
- having trouble controlling your heart rate or blood pressure.
- Diabetes type 2.
- fatty liver condition.
- imbalance of electrolytes.
- Sleep issues or circadian rhythm disturbances.
- poor body image or other negative emotional and physical impacts.
The way your hypothalamus interacts with your pituitary gland may be impacted if it sustains damage. The disease known as hypopituitarism, in which the pituitary gland produces insufficient amounts of one or more hormones, is frequently seen in individuals with hypothalamic obesity.
Diagnosis
A patient may initially seek medical attention because to worries about weight gain and the inability to reduce weight despite exercise and dietary changes. A medical expert will probably begin a diagnosis by reviewing a patient’s medical history and performing a physical examination.
Any recent head trauma or injury may be questioned by a physician. In order to look for hypothalamic injury, they could prescribe imaging studies. Hypothalamic obesity may be diagnosed by a physician if the injury occurs at the same time as rapid weight gain.
Lastly, to check for hormone levels, they could conduct a blood test. Weight gain may be the result of hypothalamic injury, as shown by abnormal hormone levels.
Once hypothalamic obesity has been diagnosed, a medical practitioner may monitor the patient and perform diagnostic testing for complications or other disorders, such as fatty liver disease and type 2 diabetes, that may arise from the condition.
Treatment of Hypothalamic Obesity
How Does Hypothalamic Obesity Affect Weight Loss?
Due to the fact that hypothalamic obesity is a “treatment-resistant” illness, conventional weight-loss strategies including behavioral and lifestyle modifications frequently fail. Symptom severity can vary, so it’s important to receive individualized care from a skilled, multidisciplinary team. It’s common for multiple problems to require simultaneous attention. Occasionally, treatments include medications and gastric bypass surgery.
Professional assistance must be sought. Your primary care physician may recommend the following experts based on the needs of your particular case:
Endocrinologist
Treatment of hormone and endocrine gland malfunction is the specialty of this kind of physician. They will assess the findings of blood tests and decide whether hormonal therapy is necessary. Thyroid hormone supplements may assist speed up metabolism, while insulin therapy can help control weight gain and keep blood sugar levels within normal ranges. If the patient is a youngster, the endocrinologist will also discuss any potential problems associated to puberty and any growth hormone deficits that may be present.
Physical Therapist
Being physically active every day is crucial. Even the most driven person might be hampered by worn-outness from inadequate sleep and low energy from a disrupted metabolism. A physical therapist will evaluate mobility, flexibility, balance, strength, and joint health. Once they have gathered this data, they can assist you in developing and following a reasonable fitness regimen. Walking and light hand weight lifting are examples of easy, low-impact workouts that might improve program success.
Dietitian
It’s critical to regulate the kinds and quantity of food consumed. Blood glucose levels will rise when simple sugars and carbs are consumed, making it more difficult to control appetite. A dietitian can help you plan nutritious meals and snacks ahead of time and educate you about food labels, which will make it simpler to make informed decisions.
Surgeon
Even with rigorous treatment, a weight loss surgeon may be required. As a last option, surgery can be required. In cases with hypothalamic obesity, the Roux-en-Y gastric bypass procedure is more effective than lap band or gastric sleeve procedures. The bypass, sometimes known as “bariatric surgery,” shrinks the stomach into a tiny pouch. The gut is then directly connected to the pouch. There are less calories consumed and absorbed since the pouch can’t contain as much food, so it “bypasses” the majority of the stomach.
An multidisciplinary team is essential for management, as mentioned. Few approved drugs are available at the moment. Although there is little research on hypothalamic obesity because it is uncommon, a number of medications have showed promise:
- Hyperphagia has been shown to improve with carbetocin (Duratocin).
- Stimulant medications like dextroamphetamine (Adderall) and a mix of caffeine and ephedrine enhance energy expenditure and reduce hunger.
- Combining the hormone oxytocin with the drug naltrexone (Vivitrol), which is commonly used to treat substance misuse, may increase feelings of fullness and reduce food obsession.
- It has been discovered that setmelanotide (Imcivree) decreases appetite and body weight in one genetic form of hypothalamic obesity.
- According to studies, a combination of metoprolol, which is mostly used to treat hypertension, and tesofensine, a neurologic medication, significantly reduced weight. The combination has the Tesomet brand.
If Untreated, What Happens?
A variety of outcomes may arise from the syndrome, depending on the underlying etiology, the degree of weight increase, and individual characteristics.
Cardiovascular Disease: The risk of cardiovascular disease, which includes high blood pressure, high cholesterol, and coronary artery disease, can be raised by excessive weight gain.
Type 2 Diabetes: It is a long-term metabolic disease marked by elevated blood sugar levels cause by improper insulin utilization by the body.
Sleep Apnea: Sleep apnea, a disorder marked by breathing pauses while you sleep, is associated with an increased risk of developing hypothalamic obesity.
Joint Problems: Osteoarthritis and joint discomfort can result from excessive weight gain because it puts more strain on the joints.
Depression and Anxiety: The development of anxiety and sadness may be exacerbated by hypothalamic obesity, which might have a substantial psychological influence.
Reduced Quality of Life: Social functioning, self-esteem, and overall well-being are all aspects of a person’s quality of life that can be greatly influenced by hypothalamic obesity.
For those with HyOb, what should I eat?
For this illness, there is no one-size-fits-all diet regimen. To find out what foods are best for you, you will consult a dietitian or nutritionist. Most people will need to consume fewer processed foods (desserts and prepackaged foods) and more nutrient-dense foods (vegetables, lean meats, and whole grains), though everyone is different.
Can you prevent HyOb?
It is caused by stress, injuries, and tumors, therefore no, you cannot prevent it. To lower your risk, however, you can do the following:
- To prevent brain damage, use a helmet and protect your head.
- receiving regular medical attention. Regularly visiting a doctor is an excellent method of identifying health issues.
Prognosis
In the event of hypothalamic obesity, what to anticipate?
Hypothalamic obesity is a very difficult condition. Since there isn’t a cure, managing your symptoms and enhancing your quality of life frequently entails close collaboration with your healthcare team. It can be discouraging to try conventional obesity therapies and discover they are ineffective. Recognize that nothing you did or didn’t do is causing your problems. Seek the help you require in close collaboration with your medical professionals, even if that support entails discussing coping mechanisms with a psychologist.
Living With When should I schedule a visit with my doctor?
Get in touch with your doctor if you experience hypothalamic obesity symptoms, such as rapid weight gain and hunger. If you have a tumor in your hypothalamus or have just suffered a head injury, this is very crucial.
Outlook
The objective is to avoid the health issues associated with obesity that can arise from this condition and affect a child’s quality of life. Hypertension, sleep apnea, joint pain, aberrant sex hormone production, diabetes, nonalcoholic fatty liver disease, and an unusually high blood fat or lipid concentration (high cholesterol or hyperlipidemia) are some examples of these consequences. The clinical team collaborates with each family to develop a customized plan of early and ongoing interventions because of this.
Children with hypothalamic obesity benefit from treatments that restrict excessive weight growth and/or lower the prevalence of obesity-related health issues in the long run. Early detection and treatment of health issues linked to obesity are also crucial. Assessment of psychological requirements that may accompany hypothalamic obesity is also beneficial for children with this illness and their families.
Conclusion
A complex issue, hypothalamic obesity is frequently linked to underlying medical disorders or hypothalamic injury. Uncontrollably gaining weight and having trouble using conventional weight loss techniques are its defining characteristics. The disorder may manifest as insulin resistance, hormonal abnormalities, and hyperphagia, among other clinical and endocrinological symptoms.
Hypothalamic obesity can be treated with a multidisciplinary strategy that includes hormone replacement treatment, diet, exercise, medication, bariatric surgery, and addressing the underlying cause of the problem. The consequences of hypothalamic obesity can be severe, and in order to avoid long-term health issues, careful management and continuous medical assistance may be necessary, even with current treatment choices.
Regardless of the cause—genetics or injury to the hypothalamus—hypothalamic obesity is a dangerous disorder that can be extremely challenging to cure. It is more likely that a skilled, interdisciplinary team will provide treatment for long-term weight loss. As long as research continues, there is hope for the future.
Hypothalamic obesity is the term used to describe fast weight gain after hypothalamic injury. Either a head injury or a brain tumor could cause the damage.
A physician may use imaging tests to determine whether a patient has suffered hypothalamic damage in order to diagnose the problem when it manifests. There isn’t a specific treatment for hypothalamic obesity at the moment, however managing weight growth and treating any underlying disorders may help mitigate the issue.
FAQs
Is It Possible for Hypothalamic Obesity to Develop in Adults and Children?
Disturbances in the hypothalamus can cause dysregulation of hunger, energy expenditure, and weight control systems, which can result in hypothalamic obesity in both children and adults.
What is the diagnosis of hypothalamic obesity?
A patient’s medical history, physical examination, growth pattern evaluation, hormone levels, imaging testing (MRI), and exclusion of other obesity-causing factors are all used to diagnose hypothalamic obesity.
Which Treatment Options Are Available for Hypothalamic Obesity Management?
The management of hypothalamic obesity may involve hormone therapy, dietary changes, behavioral therapies, increased physical activity, appetite-regulation drugs, and, in extreme situations, surgical procedures such bariatric surgery.
Could Hypothalamic Obesity Be Reversible?
Due to underlying hypothalamic dysfunction, hypothalamic obesity can be difficult to reverse; nevertheless, some degree of weight loss may be possible with comprehensive therapies, such as lifestyle modifications and medicinal treatments.
Does the Treatment of Hypothalamic Obesity Have Its Own Drug Design?
There aren’t any drugs designed especially to treat hypothalamic obesity yet. However, several medications that target metabolic processes and appetite regulation may be utilized off-label as part of therapeutic regimens.
What Lifestyle Modifications Help Manage Hypothalamic Obesity Better?
The following lifestyle changes can help manage hypothalamic obesity: eating a balanced diet, getting more exercise, controlling portion sizes, managing stress, getting enough sleep, and getting help from medical professionals.
How Does General Well-Being Get Affected by Hypothalamic Obesity?
Hypothalamic obesity can have a substantial effect on general health by raising the risk of a number of illnesses, such as diabetes, heart disease, mental anguish, and a lower quality of life.
What Issues Are Linked to Obesity in the Hypothalamus?
The following complications can lower quality of life and raise the chance of death: cardiovascular disease, type 2 diabetes, hypertension, dyslipidemia, sleep apnea, infertility, depression, and decreased mobility.
What Long-Term Effects Does Hypothalamic Obesity Have?
If treatment is not received, the long-term effects of hypothalamic obesity may include psychological effects, decreased quality of life, diabetes, and chronic health disorders like cardiovascular disease.
Can Additional Health Issues Be Caused by Hypothalamic Obesity?
Given its effects on hormonal and metabolic control, hypothalamic obesity can indeed lead to a number of health issues, such as cardiovascular disease, type 2 diabetes, hypertension, sleep disturbances, infertility, and psychological anguish.
Is Hypothalamic Obesity Associated With Any Specific Medical Conditions?
Indeed, there are a number of medical diseases that can be linked to hypothalamic obesity, including brain tumors, head trauma, genetic illnesses, and certain congenital conditions that affect the pituitary or hypothalamus.
Reference
- Hypothalamic Obesity (HYOB). (2024, October 4). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/hypothalamic-obesity
- Philadelphia, C. H. O. (n.d.). Hypothalamic obesity. Children’s Hospital of Philadelphia. https://www.chop.edu/conditions-diseases/hypothalamic-obesity
- Fletcher, J. (2023b, May 4). What to know about hypothalamic obesity. https://www.medicalnewstoday.com/articles/hypothalamic-obesity
- Mohamed, S. (2023, September 19). What is hypothalamic obesity? https://www.icliniq.com/articles/endocrine-diseases/hypothalamic-obesity