Hypoventilation
Introduction
Hypoventilation is a condition characterized by inadequate breathing, leading to increased carbon dioxide (CO₂) levels in the blood. It can result from neuromuscular disorders, obesity (obesity hypoventilation syndrome), lung diseases, or central nervous system depression.
Symptoms may include fatigue, shortness of breath, headaches, and, in severe cases, respiratory failure. Treatment depends on the underlying cause and may involve lifestyle changes, respiratory support, or medical therapy to improve ventilation and gas exchange.
Breathing too slowly or shallowly causes respiratory depression (hypoventilation), which raises blood carbon dioxide levels (hypercapnia). Respiratory depression can be caused by an overdose of some drugs, such as opioids, as well as certain disorders of the brain, lungs, and muscles. There could be difficulty breathing or an arrest of the heart.
Breathing too slowly or shallowly causes hypoventilation, which keeps your body from absorbing adequate oxygen and releasing enough carbon dioxide.
What is hypoventilation, or respiratory depression?
Breathing too slowly or shallowly can cause respiratory depression, also known as hypoventilation, which stops your lungs from properly exchanging gases. The movement of carbon dioxide (CO2) from your blood to your lungs and oxygen from your lungs’ air sacs (alveoli) to your blood is known as gas exchange. When you exhale, the CO2, a waste product that your body cannot use, subsequently exits your body.
A condition known as hypoventilation occurs when breathing is too slow or shallow to satisfy the body’s demands. As a result, blood levels of oxygen drop, and carbon dioxide builds up.
Carbon dioxide builds up in your blood due to hypoventilation, which stops it from exiting (hypercapnia). Additionally, it can occasionally stop oxygen from reaching your lungs, which can result in hypoxemia or low blood oxygen levels.
A condition known as hypoventilation occurs when breathing is too slow or shallow to satisfy the body’s demands. As a result, blood levels of oxygen drop, and carbon dioxide builds up.
Hypoventilation can have several causes, such as:
- Medical conditions: Several illnesses can impact the respiratory system and cause hypoventilation, including stroke, obesity hypoventilation syndrome, and chronic obstructive pulmonary disease (COPD).
- Drugs: When used in excess or combination with other depressants like alcohol, certain drugs, such as benzodiazepines and opioids, can depress the respiratory system and result in hypoventilation.
- Other elements: Chest wall abnormalities, neuromuscular diseases, and sleep apnea are further causes of hypoventilation.
You should get medical help right away if you think you or someone you know might be suffering from hypoventilation. Depending on the underlying reason, hypoventilation may be treated with oxygen treatment, pharmaceutical changes, or, in extreme situations, mechanical ventilation.
Causes
- Medication: Some drugs can slow down breathing by depressing the central nervous system. These drugs include barbiturates, benzodiazepines, and opioids like morphine and oxycodone. The risk of hypoventilation can be greatly increased by taking these drugs in excess or by combining them with other depressants, such as alcohol.
- The sleep disease known as obstructive sleep apnea (OSA) results in breathing pauses during sleep because the throat muscles relax and obstruct the airway. These pauses may cause hypoventilation and a drop in blood oxygen levels.
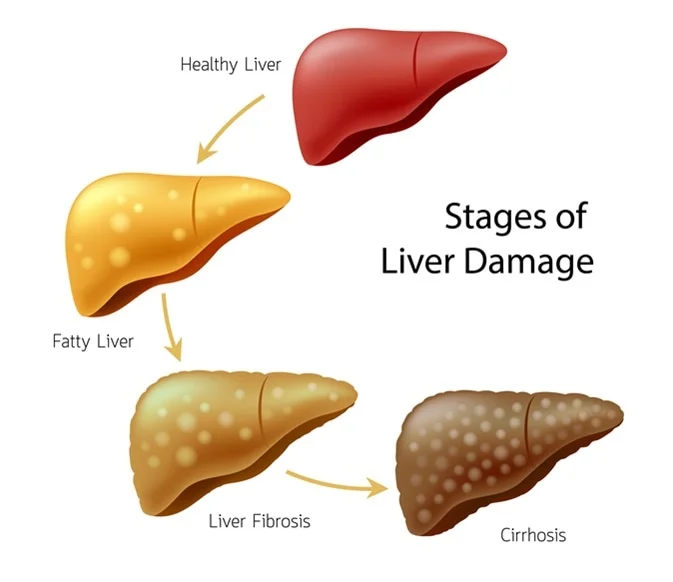
- The degenerative lung condition known as chronic obstructive pulmonary disease (COPD) destroys the lungs’ airways and air sacs, making breathing challenging. Hypoventilation can result from severe COPD, particularly when you sleep or exercise.
- Being overweight People with extreme obesity are susceptible to hypoventilation syndrome (OHS), which is typified by hypoventilation during the day. The diaphragm and chest wall may become constrained by the extra weight, making deep breathing more difficult.
- Neuromuscular Disorders: Diseases such as myasthenia gravis, muscular dystrophy, and amyotrophic lateral sclerosis (ALS) can impair the breathing muscles, resulting in hypoventilation.
- Chest Wall Deformities: Breathing difficulties and lung expansion restriction caused by kyphosis, scoliosis, and other chest wall deformities may result in hypoventilation.
- Disorders of the Central Nervous System: Hypoventilation can result from damage to the brain’s respiratory control centers caused by stroke, brain injury, and other neurological illnesses.
- Other Factors: Children’s sleep apnea, hypothyroidism, and specific genetic disorders are additional possible causes of hypoventilation.
It’s crucial to remember that hypoventilation can be a dangerous and even fatal illness. Get medical help right away if you suffer from symptoms like headaches, exhaustion, blue skin, shortness of breath, or confusion.
Hypoventilation, or respiratory depression, manifests as the following symptoms:
- Vomiting and nausea.
- A headache.
- Weariness or sluggishness.
- Perplexity, disorientation, or a change in mental state.
- Elevated heart rate.
- Lightheadedness.
- Breathing that is laborious, shallow, or slow.
- Nail, lip, or skin bluishness (cyanosis).
The most typical sign of hypoventilation is dyspnea or shortness of breath. Even with effort, you could feel as though you aren’t getting enough air.
- Fatigue: Even after taking a break, you could still feel lethargic and exhausted.
- Headache: Particularly in the morning, hypoventilation can result in headaches.
- Lightheadedness or dizziness: When you stand up rapidly, you may have lightheadedness or dizziness.
- Confusion or trouble focusing: Hypoventilation can impair mental clarity and make it challenging to concentrate or think clearly.
- Cyanosis, or bluish skin: In extreme situations, hypoventilation can result in bluish skin, particularly around the lips and fingertips. This indicates that the blood oxygen levels are low.
- Rapid heart rate: As your body attempts to make up for the low oxygen levels, your heart may beat more quickly than usual.
- Vomiting or feeling queasy: If you have severe hypoventilation, you may vomit or feel queasy.
- Seizures: Hypoventilation can occasionally result in seizures.
It’s crucial to remember that the underlying cause of hypoventilation and the general health of the person can affect how severe the symptoms are. It’s critical to consult a physician if you encounter any of these symptoms to receive a diagnosis and treatment strategy.
Other considerations about the symptoms of hypoventilation are as follows:
- The symptoms could worsen while you’re sleeping or at night.
- Exertion may exacerbate symptoms.
- Some hypoventilation sufferers might not exhibit any symptoms at all.
It is crucial to have a medical professional evaluate you if you are worried about hypoventilation. Serious consequences can be avoided with early identification and treatment.
Why does respiratory depression occur?
Respiratory depression is frequently caused by alcohol abuse, overdose, or an unanticipated reaction to prescription pharmaceuticals, alcohol, or other substances, such as:
- Opioids. Common opioids, sometimes known as narcotics, include oxycodone, fentanyl, Vicodin®, and morphine.
- Benzodiazepines. Lorazepam, alprazolam, and diazepam are a few examples of common benzodiazepines.
- Barbiturates. Barbiturates are occasionally administered to treat migraines or seizures.
- Medications that are not medicinal. This includes gamma hydroxybutyrate (GHB) and heroin.
- Prescription sleep aids. This includes Ambien’s zolpidem.
- Anesthesia.
Hypoventilation can also result from the following other illnesses and conditions:
- Experiencing obesity (also known as obesity hypoventilation syndrome or OHS).
- Circumstances that make it difficult for you to breathe. This includes obstructive sleep apnea and chronic obstructive pulmonary disease (COPD).
- Circumstances that impair your respiratory drive, or capacity to control your breathing. Hypothyroidism and stroke are two examples.
- Disorders that impact your nerves, muscles, or spinal cord. Multiple sclerosis (MS), amyotrophic lateral sclerosis (ALS), muscular dystrophy, and damage to the nerves or spinal cord are a few examples.
- Variations in the structure of the spine or chest. Examples include flail chest, ankylosing spondylitis, and scoliosis.
- Poisoning or poisoning. Some examples include botulism, tetanus, and ciguatera toxicity, which is poisoning from infected fish.
Which factors increase the likelihood of respiratory depression?
Among the risk factors associated with respiratory depression are:
Abuse of prescription or over-the-counter medications, such as benzodiazepines or opioids. Certain neurological (which consists of and spinal cord), muscular, and lung disorders, such as those mentioned above.
Because of the accumulation of carbon dioxide in the blood and the consequent drop in oxygen levels, hypoventilation can cause several dangerous problems if treatment is not received. The following are a few of the biggest issues:
When there is too much carbon dioxide in the blood, it causes respiratory acidosis. This may interfere with several body processes and cause more issues.
Respiratory failure is a potentially fatal illness in which the lungs are unable to sufficiently expel carbon dioxide from the body or supply oxygen to it. To maintain breathing, mechanical ventilation is frequently needed.
- Cardiac Arrest: When hypoventilation is severe, the heart may cease beating normally, a condition known as cardiac arrest. This is a health problem that requires immediate attention.
- Coma: Because oxygen cannot reach the brain during prolonged and severe hypoventilation, a person may lose consciousness and enter a coma.
- Pulmonary Hypertension: A condition known as pulmonary hypertension is caused by persistent hypoventilation, which raises blood pressure in the lungs’ arteries. Heart failure may result from this strain on the heart.
- Brain Damage: Because severe hypoventilation deprives the brain of oxygen, it can result in irreparable brain damage. Seizures, cognitive decline, and other neurological issues may result from this.
- Death: Hypoventilation can be lethal in the worst situations. This is particularly true if it is not identified and treated every once, or if a drug overdose causes it.
It’s critical to get medical help right away if you or someone you love is exhibiting signs of hypoventilation, such as headache, lethargy, bluish skin, shortness of breath, or confusion. Treatment and identification at an early stage can help avoid these potentially fatal consequences.
What side effects might respiratory depression cause?
Life-threatening consequences can result from elevated blood carbon dioxide levels, including:
- Breathing acidosis. Your blood has become greater corrosive than it should be in this condition.
- Respiratory malfunction. In this scenario, your body’s tissues are unable to receive adequate oxygen.
- Cardiac arrest.
- Coma.
- Hypertension of the lungs.
Testing and Diagnosis
How is hypoventilation, or respiratory depression, diagnosed?
A healthcare professional will inquire about your symptoms, medical history, and current medications to identify respiratory depression. To detect the amount of carbon dioxide in your blood, they could employ specialized blood tests. To determine the reason for hypoventilation, they could additionally employ other testing.
Which tests could be applied?
The following tests are used to identify respiratory depression and its underlying causes:
- Test for arterial blood gas.
- Testing for pulmonary function.
- Oximetry of the pulse. The amount of oxygen in your blood is measured by providers using a sensor that fits over your finger.
- Blood examinations. Numerous blood tests are useful in the diagnosis of respiratory depression and its underlying causes. These could include a thyroid function test, CO2 blood test, toxicological screen, basic metabolic panel (BMP), and full blood count (CBC).
- Picture. A physician may obtain CT scans (computed tomography scans) of your head or chest or chest X-rays to assist in identifying any underlying issues.
- Sleep research (polysomnography).In addition to evaluating obese hypoventilation syndrome, which can result in hypoventilation, a sleep study can identify sleep apnea.
Handling and Therapy
How is hypoventilation, or respiratory depression, treated?
The origin and severity of respiratory depression determine the course of treatment. Medical professionals might provide you:
- Noninvasive ventilation. This device assists you in breathing through a face mask. Bilevel positive airway pressure and continuous positive airway pressure (CPAP) are two examples.
- Drugs that stimulate the respiratory system. If respiratory depression is the result of an overdose or adverse consequence, a physician may be able to reverse it with reversal agent drugs. As a reversal agent, naloxone (Narcan®) can undo the effects of opioids.
- Oxygen treatment.
- Ventilation using mechanical means.
- Addressing the underlying cause: It’s critical to address any underlying medical conditions that may be contributing to hypoventilation, such as sleep apnea, COPD, or a neuromuscular disease. This could entail lifestyle modifications, treatment, or medication.
- Drugs: In certain situations, drugs may be used to help with breathing. Respiratory stimulants, for instance, can aid in accelerating and deepening breathing. These drugs can have adverse effects and aren’t always effective.
- Oxygen therapy: Additional oxygen may be given via a mask or nasal cannula if hypoventilation results in low blood oxygen levels.
This lowers symptoms and raises oxygen levels.
- Non-invasive ventilation: Non-invasive ventilation methods may be employed in more serious situations. To maintain open airways and enhance breathing, these methods use a machine to apply air pressure through a mask. Bilevel positive airway pressure (BiPAP) and continuous positive airway pressure (CPAP) are two examples.
- Mechanical ventilation: This treatment may be required in the most severe hypoventilation instances. This entails breathing for the patient via a machine and putting a tube into the trachea. Usually, this is carried out at a hospital.
Lifestyle changes:
Lifestyle changes can sometimes help with hypoventilation. This could entail abstaining from alcohol and sedatives, maintaining proper sleep hygiene, and decreasing weight if obesity is a contributory issue.
It’s crucial to remember that each person’s needs should be taken into consideration when treating hypoventilation. A medical expert will choose the best course of action depending on the condition’s severity, underlying cause, and other considerations.
You must get medical help right away if you’re having hypoventilation symptoms. Serious consequences can be avoided with early identification and treatment.
Avoidance
Is it possible to avoid respiratory depression?
Taking prescription drugs as directed and taking care of any underlying medical issues are the best ways to avoid respiratory depression. Before using two or more drugs together, especially benzodiazepines, opioids, or other sedatives, see your doctor or pharmacist. Additionally, be mindful of potential drug-alcohol interactions.
Prognosis and Outlook
What is the respiratory depression prognosis?
The etiology of respiratory depression determines the prognosis. If not addressed right away, emergency conditions like an opioid overdose can be lethal. You may eventually get unwell from other causes, such as sleep apnea, OHS, or chronic illnesses, and require continuous care.
What time should I visit my doctor?
Speak with your physician if:
- You have queries or worries regarding a health issue you have.
- Regarding a prescription drug, you have queries or worries.
- You exhibit respiratory depression signs, particularly if you also have another risky illness.
When should I visit the emergency room?
If you exhibit any of the following symptoms of a serious disease, visit the closest emergency room:
- Seizures.
- Bewilderment or a change in mental state.
- Unable to remain conscious.
- Confusion.
- Paranoia.
- Blue lips, skin, or nails.
What alternatives do I have for treatment?
A dangerous illness called respiratory depression causes carbon dioxide to accumulate in the blood. However, it is often avoidable. Consult your doctor to ensure you are taking your meds as prescribed if you are at risk for respiratory depression.
Ask your doctor what precautions you can take if you have a chronic illness that can lead to respiratory depression. They can discuss your worries with you and come up with a plan to carefully manage your condition or drugs.
FAQs
In nursing, what distinguishes hyperventilation from hypoventilation?
Prolonged bed rest, a client’s reluctance to breathe regularly when breathing hurts, or an excess of some medications can all result in hypoventilation. In contrast, carbon dioxide is expelled from the body more quickly than it is produced when hyperventilation occurs, which is defined as breathing that is overly deep or rapid.
Is hypoventilation a symptom of asthma?
Obesity hypoventilation syndrome, neuromuscular illnesses, obstructive lung diseases (such as asthma or chronic obstructive lung disease), and the use of pharmaceuticals or medications that might reduce respiratory drive can all cause hypoventilation.
What is the effect of hypoventilation on blood pH?
Carbon dioxide buildup and ventilation failure are the usual causes of respiratory acidosis. The main disruption is a drop in the ratio of arterial bicarbonate to arterial pCO2 and an increase in arterial partial pressure of carbon dioxide (pCO2), which lowers blood pH.
What does hypoventilation look like?
Hypoventilation can result from sleep apnea, a condition in which a person repeatedly stops breathing while they are asleep. In rare instances, the reason for hypoventilation may not be understood, and an examination reveals an unobstructed airway. SIDS, or sudden infant death syndrome, is one instance of this.
What other names are there for hypoventilation?
Rapid or deep breathing, commonly caused by stress or worry, is known as hyperventilation. You might truly feel out of breath from this so-called over-breathing. You take in oxygen and release carbon dioxide as you breathe.
How is a diagnosis of hypoventilation made?
Chest radiography, pulmonary function testing, clinical history, and physical examination are all necessary when evaluating a patient who has hypoventilation to identify the etiology. It might also be necessary to undergo specialized testing, such as evaluating ventilatory control and measuring respiratory muscle strength.
Which medications result in respiratory depression?
Benzodiazepines, like midazolam or diazepam, might raise the risk of respiratory depression, especially when used with other psychiatric medications like antidepressants, antipsychotics, anticonvulsants, or sedatives like phenobarbital.
What heart rate is ideal?
Adults’ resting heart rates usually range from sixty beats to one hundred per minute. Generally speaking, a decreased resting heart rate indicates better cardiac function and cardiovascular fitness. A well-trained athlete, for instance, may have a resting heart rate that is more in line with 40 beats per minute.
Reference
- Respiratory depression (Hypoventilation). (2024, December 19). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/respiratory-depression
- Hypoventilation: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/002377.htm#:~:text=Hypoventilation%20is%20breathing%20that%20is,with%20hypoventilation%20might%20feel%20sleepy.