Diabetes And Obesity Management
Introduction
Obesity and diabetes are two chronic diseases that are closely associated and have grown to be significant global health issues. One important risk factor for the onset of type 2 diabetes is the rising incidence of obesity. To avoid problems, enhance quality of life, and lower healthcare expenses, both illnesses must be well managed.
A multimodal strategy involving behavioral adjustments, medication, and lifestyle changes is necessary for the effective management of diabetes and obesity. To control blood sugar levels and achieve long-term weight loss, diet, exercise, and medication are essential. Furthermore, new developments in medical care, such as drugs like GLP-1 receptor agonists and metabolic surgery, give people with both disorders fresh hope.
The complex relationship between diabetes and obesity is examined in this article, which also highlights evidence-based care and preventative techniques. People can take proactive measures to improve their health and quality of life by being aware of these interrelated diseases.
Diabetes
Diabetes is a metabolic disease marked by elevated blood sugar levels caused by either insufficient insulin synthesis or insulin resistance. Among the primary forms of diabetes are:
Type 1 diabetes is an autoimmune disease in which the body’s immune system targets the pancreatic cells that produce insulin. Insulin treatment is necessary.
The most prevalent type of diabetes is type 2, in which the body either produces insufficient insulin or becomes resistant to it. It is frequently connected to lifestyle elements like food and exercise.
Pregnancy causes gestational diabetes, which raises the chance of Type 2 diabetes in the future.
Effects of Diabetes
- Over time, high blood sugar can harm tissues and organs.
- Raises the chance of kidney failure, nerve damage, heart disease, and eyesight loss.
- Calls for medication, lifestyle modifications, and ongoing observation.
Obesity
Excessive fat accumulation that poses health problems is referred to as obesity. Body Mass Index (BMI) is frequently used to quantify it; an individual is deemed obese if their BMI is 30 or over. Obesity raises the risk of heart disease, type 2 diabetes, and several types of cancer, among other illnesses.
Excess body fat, which is commonly assessed using the Body Mass Index (BMI), is what defines obesity:
- Obese people have a body composition index (BMI) of thirty or more.
- A BMI of 25–29.9 indicates overweight.
Causes of Obesity
- Poor diet (high-calorie, processed foods).
- Sedentary lifestyle.
- Genetic factors.
- Hormonal imbalances.
- Certain medications.
The Risks of Obesity to Health
- Raise the risk of heart disease, stroke, hypertension, and Type 2 diabetes.
- Can result in mental health difficulties, sleep apnea, and joint problems.
- Impacts living quality in general.
The Connection Between Diabetes and Obesity
One of the main risk factors for type 2 diabetes is obesity. Metabolic dysfunction, inflammation, and insulin resistance are all exacerbated by excess fat, especially visceral fat. The interplay between obesity and diabetes can lead to severe complications such as neuropathy, kidney disease, and cardiovascular issues.
Obesity and diabetes are two of the most common health issues in the world, and there is ample evidence linking the two. Excessive body fat buildup is a hallmark of obesity, which raises the risk of Type 2 diabetes, a metabolic disease that interferes with blood sugar homeostasis. The body finds it more difficult to properly regulate glucose when there is extra fat, especially around the belly, which leads to insulin resistance.
The word “diabesity” was created to characterize their coexistence because of how strongly they are related. Prevention and management of diabetes and obesity depend on an understanding of the underlying mechanisms that link these two illnesses. This article examines the complex relationship between diabetes and obesity, illuminating the risks, causes, and possible countermeasures.
Strategies for Management
Changes in Lifestyle: Dietary Adjustments: Blood sugar regulation and weight management are aided by a balanced diet high in fiber, lean proteins, healthy fats, and complex carbohydrates. One of the best strategies to control weight, avoid chronic diseases, and enhance general health is to make dietary modifications. Making dietary changes can have a big influence on your well-being, whether your goal is to eat healthier, reduce weight, or treat a particular health issue.
Smaller adjustments like cutting back on sugar or eating more fruits and vegetables are examples of dietary changes, as are more substantial ones like switching to a plant-based diet or adhering to a particular eating plan (such as the Mediterranean or ketogenic diets).
Making sustainable food and habit choices that fit your lifestyle and can be sustained over time is the key to effective dietary adjustments. Compared to severe, short-term diets, gradual modifications frequently result in better adherence and long-lasting effects.
Including mindful eating, balanced nutrition, and adequate water in daily routines can help enhance mental clarity, energy levels, and digestion. Whatever your objective, developing a better connection with food will be facilitated by knowing the fundamentals of nutrition and making wise decisions.
Physical Activity: Consistent exercise, such as strength training and aerobic exercises, increases insulin sensitivity and aids in weight loss. Two of the most common chronic illnesses in the world, diabetes, and obesity, can be prevented and managed in large part via physical activity. Because too much body fat can result in insulin resistance and metabolic abnormalities, obesity is a major risk factor for type 2 diabetes. Frequent exercise is an important part of diabetes and obesity treatment plans because it helps control blood glucose levels, enhance insulin sensitivity, and promote weight management.
Exercise improves mental health, lowers the risk of cardiovascular illnesses, and encourages a healthy lifestyle in addition to its physiological advantages. This study examines the relationship between physical activity and the management of diabetes and obesity, emphasizing the efficacy of evidence-based exercise regimens in managing these illnesses.
Behavioral Therapy: Long-term weight and glucose control is facilitated by behavioral changes, goal-setting, and psychological support. Obesity and diabetes are two of the most common chronic illnesses in the world. They frequently coexist and can lead to serious side effects such as metabolic abnormalities, cardiovascular disease, and a lower quality of life. Behavioral therapy has become a vital part of successful treatment, even while pharmaceutical and medical therapies are important in managing these diseases. The main goals of behavioral therapy are to improve self-care practices, change bad habits, and encourage long-term lifestyle adjustments that help with blood sugar regulation and weight management.
Behavioral therapies assist people in creating long-lasting changes in their nutrition, level of physical activity, and stress management by employing methods including cognitive-behavioral therapy (CBT), motivational interviewing, and habit formation tactics. These methods work especially well for treating sedentary behavior, emotional eating, and other lifestyle issues that lead to both.
Medical Management
Diabetes medications include SGLT2 inhibitors, GLP-1 receptor agonists, metformin, and insulin therapy, which all aid in blood sugar regulation.
Diabetes is a long-term illness that alters the body’s ability to control blood sugar or glucose. Diabetes management frequently calls for a mix of medication, lifestyle modifications, and monitoring. Diabetes drugs aid in blood sugar regulation and the avoidance of consequences such as renal failure, heart disease, and nerve damage.
Diabetes comes in two primary forms:
- Insulin therapy is necessary for people with type 1 diabetes since their bodies are unable to manufacture insulin.
- Type 2 Diabetes: Usually treated with insulin, injectable meds, or oral medications, this condition is caused by the body’s ineffective use of insulin.
Diabetes drugs function in a variety of ways, such as:
- promoting the synthesis of insulin (e.g., meglitinides, sulfonylureas)
- Increasing insulin sensitivity (e.g., thiazolidinediones, metformin)
- decreasing the absorption of glucose (e.g., SGLT2 inhibitors, alpha-glucosidase inhibitors)
- GLP-1 receptor agonists, for example, slow appetite and digestion.
- Directly replacing insulin (different kinds of insulin)
The type of diabetes, blood sugar levels, lifestyle, and general health all influence the medication decision. Effective diabetes management requires routine monitoring and adaptation.
Diabetes and obesity are major global health issues that hurt general health and raise the risk of several consequences, such as metabolic disorders, hypertension, and cardiovascular disease. Effective management of these disorders frequently calls for a mix of pharmaceutical treatments and lifestyle changes, such as dietary and activity changes.
Numerous drugs have been created to help with glycemic control and weight management. These medications function via several pathways, including reduction of fat absorption, glucose control, and appetite suppression. GLP-1 receptor agonists and SGLT-2 inhibitors are two novel medicines that have been made possible by recent developments in pharmacology. These drugs have shown great promise in the treatment of diabetes and weight loss.
The piece examines the many drug classes for managing weight, diabetes, and obesity, as well as their benefits, possible disadvantages, and modes of action. Patients and healthcare professionals must be aware of these treatment alternatives to make well-informed decisions about the appropriate management of these chronic illnesses.
Surgical Interventions
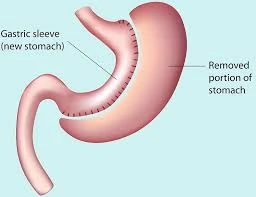
Bariatric Surgery: For people who are extremely obese, procedures such as gastric bypass and sleeve gastrectomy greatly help with weight loss and blood sugar regulation.
An extremely successful treatment for people with obesity and obesity-related diseases, especially type 2 diabetes, is bariatric surgery. In addition to promoting substantial weight loss, this surgical technique is essential for enhancing metabolic health, which frequently results in diabetes remission or less reliance on medication.
Given that obesity is still a major global health concern and is closely associated with diabetes and other chronic illnesses, bariatric surgery presents a viable option for those who have failed to lose weight sustainably using traditional strategies like diet and exercise.
Preventive Measures
Public health initiatives: Community-based interventions, nutrition education, and awareness campaigns promote healthy living.
Two of the most important global public health issues are diabetes and obesity, which raise healthcare expenses, lower quality of life, and increase the risk of chronic diseases like cardiovascular disease. By putting preventative measures into place, encouraging healthy lifestyles, and guaranteeing access to medical treatment, public health programs play a critical role in combating these epidemics.
Numerous interventions have been started by governments, healthcare institutions, and community-based initiatives. These include nutritional education, physical activity promotion, public awareness campaigns, and regulatory reforms like sugar levies and food labeling laws. These programs seek to enhance early identification, lower the prevalence of diabetes and obesity, and improve management techniques for individuals who are already impacted.
Screening for diabetes involves monitoring blood glucose levels, identifying risk factors such as family history and lifestyle habits, and detecting prediabetes before it progresses to full-blown diabetes. Similarly, obesity screening includes measuring body mass index (BMI), and waist circumference, and assessing related health risks such as cardiovascular disease and metabolic syndrome.
Frequent Screening: Timely intervention is made possible by early detection of prediabetes and problems connected to obesity.
Two of the most common chronic illnesses in the world, diabetes and obesity, have a substantial impact on morbidity, mortality, and medical expenses. Frequent screening helps people and healthcare professionals make educated decisions about treatment and lifestyle changes by assisting in the early detection, prevention, and management of various disorders.
Routine screening for early diagnosis allows for prompt action, which lowers complications and enhances overall health outcomes. This study examines the value of routine screening in the treatment of diabetes and obesity, emphasizing suggested practices, advantages, and practical implementation techniques.
Conclusion
Obesity and diabetes are closely related medical disorders that need to be managed with a multimodal strategy. A mix of behavioral adjustments, medicinal treatments, and lifestyle adjustments are needed to address these problems. Improving insulin sensitivity and lowering the risk of problems on weight control, frequent exercise, and a healthy diet.
Effective management of these illnesses has also been improved by developments in drugs, surgical techniques, and individualized therapy programs. To prevent and manage the rising rates of diabetes and obesity, public health programs and education are also essential.
People can greatly enhance their general well-being and lower the long-term dangers connected to these chronic diseases by taking a proactive stance and encouraging better lives. Future diabetes and obesity management techniques will be progressively strengthened by ongoing investigation and development.
FAQs
What connection exists between fat and diabetes?
One of the main risk factors for type 2 diabetes is obesity. The body finds it more difficult to control blood sugar levels when there is excess fat, particularly around the belly since it raises insulin resistance.
Can diabetes be managed with weight loss?
Even a small weight loss (5–10% of body weight) can have a major positive impact on insulin sensitivity, blood sugar regulation, and general health.
How does insulin resistance relate to obesity, and what does it mean?
High blood sugar levels are a result of insulin resistance, which happens when cells lose their sensitivity to insulin. This syndrome is exacerbated by excess body fat, particularly visceral fat.
Which foods are best avoided by those who have both diabetes and obesity?
Limit your intake of highly processed foods, sugary beverages, refined carbohydrates, and harmful fats. Rather, prioritize complete foods, veggies high in fiber, lean meats, and healthy fats.
Is it safe for diabetics to fast intermittently?
Blood sugar regulation and weight loss may be aided by intermittent fasting, but it should only be carried out under medical supervision, particularly for people taking insulin or other diabetic drugs.
If I have diabetes, how many carbohydrates should I consume each day?
Although everyone has different demands when it comes to carbohydrates, most diabetics benefit from consuming 45–60 grams every meal. Personalized advice can be given by a qualified dietician.
Which kind of exercise is most effective in controlling obesity and diabetes?
The best way to improve insulin sensitivity and weight management is to combine strength training (lifting weights, resistance exercises) with aerobic activity (walking, swimming).
Does stress have an impact on obesity and diabetes?
Indeed, long-term stress raises cortisol levels, which can result in weight gain and elevated blood sugar. Stress-reduction methods such as yoga, deep breathing, and meditation can be beneficial.
Are there drugs that can help people lose weight and manage their diabetes?
Indeed, certain drugs, such as GLP-1 receptor agonists (Ozempic, Wegovy, and Mounjaro), can aid in both blood sugar regulation and weight loss. Discuss your choices with your physician.
Is bariatric surgery a viable treatment for obesity and diabetes?
For people with type 2 diabetes and extreme obesity, bariatric surgery can be very beneficial. It frequently results in substantial weight loss and, in certain situations, even diabetic remission.
How frequently should my blood sugar be checked?
Your diabetes type and treatment strategy will determine this. While individuals on insulin may need to check more frequently, many people with type 2 diabetes only check once or twice a day.
Can losing weight reverse diabetes?
Significant weight loss, particularly through lifestyle modifications or surgery, can result in remission—normal blood sugar levels without the need for medication—for some people with type 2 diabetes.
References
- Ruze, R., Liu, T., Zou, X., Song, J., Chen, Y., Xu, R., Yin, X., & Xu, Q. (2023). Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Frontiers in Endocrinology, 14. https://doi.org/10.3389/fendo.2023.1161521
- Morissette, A., & Mulvihill, E. E. (2024). Obesity management for the treatment of type 2 diabetes: emerging evidence and therapeutic approaches. Journal of Pharmacy & Pharmaceutical Sciences, 27. https://doi.org/10.3389/jpps.2024.13065
- Sulu, C., & Yumuk, V. D. (2024). Treat obesity to treat type 2 diabetes mellitus. Diabetes Therapy, 15(3), 611–622. https://doi.org/10.1007/s13300-024-01536-3