Heart Disease
The heart is a muscular organ that contracts and expands to circulate blood throughout the circulatory system. Any condition that affects the heart or its function is considered heart disease. Cardiovascular disease is the medical term for heart disease.
The primary cause of death in the US is heart disease, according to the Centers for Disease Control and Prevention (CDC). Heart disease is responsible for almost one out of every four deaths in the United States, and it affects people of all racial and ethnic backgrounds and genders.
What is Heart Disease?
There are several types of heart disease and several problems that might impact the function of your heart. Cardiovascular disease is another name for heart disease, and it also refers to issues with blood arteries.
About 1 in 5 deaths, or 700,000 deaths annually, in the United States are attributable to heart disease.
Treatments and symptoms vary depending on the type of heart disease. Medication and lifestyle modifications can significantly impact your health if you have certain types. Others could need surgery to get their pulses working properly again.
Relevant Anatomy
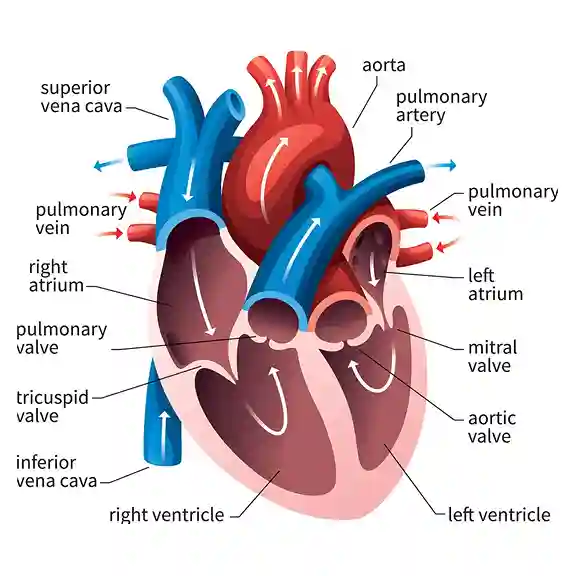
The muscular organ known as the heart is responsible for gathering deoxygenated blood from all areas of the body, transporting it to the lungs for oxygenation, and releasing carbon dioxide. After that, it distributes the oxygenated blood to every region of the body by transporting it from the lungs.
- Every day, the heart circulates about 7,200 liters of blood throughout the body.
- The heart points slightly to the left and is located in the middle of the chest.
- The heart beats roughly 100,000 times every day on average, or about 3 billion times throughout a lifetime.
- The average heartbeat for an adult is between 60 and 80 beats per minute, whereas the heartbeat of a newborn baby is between 70 and 190 beats per minute.
The pericardium encloses the heart, a conical, hollow, muscular structure located in the middle mediastinum. With one-third on the right and two-thirds on the left of the midline, it is positioned posteriorly to the sternum’s body. The heart weighs about 310 g for men and 255 g for women, and it measures 12 x 8.5 x 6 cm. To supply their nutritional needs, it circulates blood to different regions of the body. The term “cardia,” which means heart in Greek, is the root of the word “cardia.”
Relations
- Anteriorly: the left lung, pleura (apex), and the sternum’s body and surrounding costal cartilages
- Posteriorly: esophagus, descending thoracic aorta, azygos and hemiazygos veins, and thoracic duct.
- Superficially: bifurcation of the major pulmonary trunk.
- The inferior diaphragm
- Laterally: the pleura and lungs
Layers of the Heart Walls
The pericardium encloses three layers that make up the heart wall:
- The epicardium is the outermost layer of the heart’s wall, made up of the serous pericardium’s serous layer.
- The myocardium is the muscular middle layer of the heart’s wall, which contains the conducting system and excitable tissue.
- Endocardium: An intermediate concentric layer. A layer beneath the heart.
The subepicardial and subendocardial layers make up the majority of the remaining heart.
Structure and Function
The right and left halves of the heart are separated by septa, and each half is further divided into two cavities by a constriction. The upper cavity is known as the atrium, while the lower cavity is called the ventricle. As a result, the heart has four chambers:
- The right ventricle, left ventricle, right atrium, and left atrium.
The four chambers and four valves should ideally be recalled in the sequence that blood passes through the heart:
- Through the SVC, IVC, and coronary sinus, venous blood that has returned from the body empties into the right atrium.
- Blood is pumped from the right atrium into the right ventricle via the tricuspid valve.
- To get oxygen into the lungs, the right ventricle pumps blood into the pulmonary trunk via the pulmonary semilunar valve.
- The four pulmonary veins carry blood from the lungs back into the left atrium.
- Blood is pumped from the left atrium into the left ventricle via the bicuspid (mitral) valve.
- To supply the body, the left ventricle pumps blood into the ascending aorta via the aortic semilunar valve.
Heart Valves
The heart’s valves keep blood flowing just in one way and stop it from regurgitating in the other. The atrioventricular and semilunar valves are the two pairs of valves that make up the heart. It has four valves in total. The goal of the heart’s four valves is the same: to permit blood to flow forward while blocking backward flow. A heart valve protects each chamber’s outflow:
The atrioventricular valves that separate the ventricles and atria
- Tricuspid valve (heart’s right side)
- Bicuspid/mitral valve (left side of the heart)
The ventricles’ outflow pathways have semilunar valves.
- Aortic valve (heart’s left side)
- pulmonary valve (heart’s right side)
Types Of Heart Diseases
- Rheumatic Heart Disease
- Valvular Heart Disease
- Hypertensive Heart Diseases
- Cerebrovascular Heart Disease
- Inflammatory Heart Disease
- Ischemic Heart Disease
Rheumatic Heart Disease
Rheumatic fever is the cause of rheumatic heart disease, a persistent heart disorder. This heart condition is extremely prevalent in kids. The disease is more common in emerging nations, particularly in impoverished communities.
An inflammatory condition, acute rheumatic fever mostly affects the heart, joints, and central nervous system. The most frequent consequence of rheumatic fever is damage to the heart valves. The inflammation caused by rheumatic disease may harm the endocardium, which is the inner lining, and the pericardium, which is the outer sac.
Usually beginning as strep throat, rheumatic fever progresses to a fever. Taking penicillin or antibiotics can stop this development.
In the US, rheumatic heart disease is uncommon. It is particularly prevalent in underdeveloped or low-income regions of the world when individuals lack access to antibiotics for diseases caused by bacteria. Every year, rheumatic heart disease kills the lives of almost 300,000 people globally. Approximately 40 million people globally suffer from the disease.
Rheumatic fever is most common in children and teenagers with untreated strep infections, usually between the ages of 5 and 15. Years after the disease and fever have subsided, heart damage symptoms may appear. Rheumatic heart disease frequently manifests in young adults.
What symptoms of rheumatic heart disease are present?
Acute rheumatic fever episodes might cause signs of cardiac involvement in certain patients. However, symptoms of rheumatic heart disease typically do not show up until years after a rheumatic fever or strep infection. Heart injury sufferers may encounter:
- Chest pain.
- Fatigue.
- Heart murmur
- Difficulty breathing while exercising, relaxing, or lying flat.
- Swelling in your hands, feet, or stomach.
- Heart arrhythmias such as atrial fibrillation or palpitations.
- Coughing up blood.
What causes rheumatic heart disease?
Rheumatic fever induces inflammation of the heart valves, which leads to rheumatic heart disease. The damage might occur immediately. It may also develop gradually as a result of recurrent strep infections. Heart valve constriction and scarring are caused by persistent inflammation.
How is the diagnosis of rheumatic heart disease made?
A medical professional will assess your symptoms and conduct a physical examination to identify rheumatic heart disease. Your medical history will also be examined, particularly any episodes of bacterial infections or fevers.
Which diagnostic procedures will be used to identify rheumatic heart disease?
The following tests could be used by your doctor to identify rheumatic heart disease:
- Blood tests to detect a strong immune response or inflammation.
- X-ray of the chest to look for heart failure symptoms.
- An echocardiogram, or ultrasound of the heart, can detect constricted or leaking heart valves.
- An electrocardiogram (EKG), which measures the electrical activity of the heart, is used to look for irregular beats.
Management
What is the treatment for rheumatic heart disease?
Treatments for rheumatic heart disease may help you control your symptoms and slow the progression of the condition. However, they are unable to treat the disease. Among the treatments are:
Medication: To treat heart failure or an irregular heartbeat, your doctor may suggest medication. If you have atrial fibrillation or a narrow mitral valve, anticoagulants (blood thinners) can lower your risk of stroke or blood clots.
Minimally invasive procedure: A physician can do a valvuloplasty to enlarge your narrow mitral valve if you don’t have any other problems with it.
Surgery: You might require heart valve surgery if you have severe rheumatic heart disease. Damaged heart valves are replaced or repaired by a surgeon. If they are unable to repair your damaged valve, they can use a tissue valve or an artificial valve in its place. In certain situations, they might do a Ross surgery, in which a surgeon replaces the damaged valve with one of your healthy valves and then replaces the relocated healthy valve with a new one.
Valvular Heart Disease
Valvular heart disease is the result of damage to any of the heart’s valves, including the tricuspid, mitral, pulmonary, and aortic valves. Age-related deterioration of the heart valves is the primary cause of this diseases.
These valves are responsible for ensuring that blood flows in the proper direction and at the proper speed. The heart’s valves become extremely thin and rigid in valvular heart disease conditions, which alters the system’s blood flow rate and velocity. They might occasionally be closed.
Causes
Knowing the causes of heart valve diseases may be easier if you understand how the heart works. The proper flow of blood is maintained by four heart valves. The valves are as follows:
- The mitral valve
- The aortic valve
- The tricuspid valve
- The pulmonary valve
The flaps on each valve are called cusps or leaflets. The flaps open and close once with each heartbeat. Less blood flows from the heart to the body when a valve flap doesn’t open or close all the way.
Here are some types of heart valve disease:
Stenosis: The valve flaps may occasionally join together and thicken or stiffen. The valve’s opening gets smaller. Less blood can flow via the constricted valve.
Regurgitation: Blood may flow backward due to possibly loose valve flaps.
Prolapse: The flaps of the valve enlarge and become floppy. They protrude like a parachute. This disease can cause regurgitation.
Atresia: This condition is caused by improperly constructed valves, which impede blood flow between the heart’s chambers. This variation usually affects the pulmonary valve, where a solid layer of tissue obstructs the blood’s normal flow.
Signs and symptoms
For many years, some persons with heart valve dysfunction may not exhibit any symptoms. Symptoms may include the following when they manifest:
- Difficulty breathing when lying down, moving around, or at rest.
- Fatigue.
- Chest pain.
- Lightheadedness.
- Swelling in the feet and ankles.
- Fainting.
- Irregular heartbeat.
How are diseases of the heart valves treated?
Treatments for heart valve disorders that work well include:
- Drugs are designed to manage symptoms and maintain healthy heart function.
- Heart-related diseases can be prevented by adopting coronary heart-healthy lifestyle changes.
- Surgical procedures to replace or repair valves.
Remember that surgery can be recommended even if there are no symptoms since it can prevent future heart problems by fixing the underlying valve problem.
Your general health and the particular valve issue will determine which surgical treatment options are best for you. Additionally, surgery to repair a heart valve is typically preferred over valve replacement because of the decreased risks.
Hypertensive Heart Diseases
A chronic disorder that develops over many years in persons with high blood pressure is hypertensive heart disease. It’s a collection of health issues that can arise from uncontrolled high blood pressure (hypertension), including heart failure and conduction arrhythmias.
Hypertensive heart disease is caused by persistently high blood pressure (greater than 120/80 mmHg). People who continue to have high blood pressure as they age are more likely to develop heart disease. People over 65 are most likely to get heart failure.
Your heart has to work harder to pump blood when you have chronically high blood pressure. Heart failure may result from the thickening and weakening of your heart muscle. High blood pressure can also cause the walls of your blood vessels to thicken, even more harmful when cholesterol builds up inside the blood vessels. Your chances of having a heart attack or stroke then increase.
Heart failure is twice as common in men and three times as common in women with high blood pressure. However, you can significantly lower your risk of heart failure by managing your excessive blood pressure.
Aneurysm
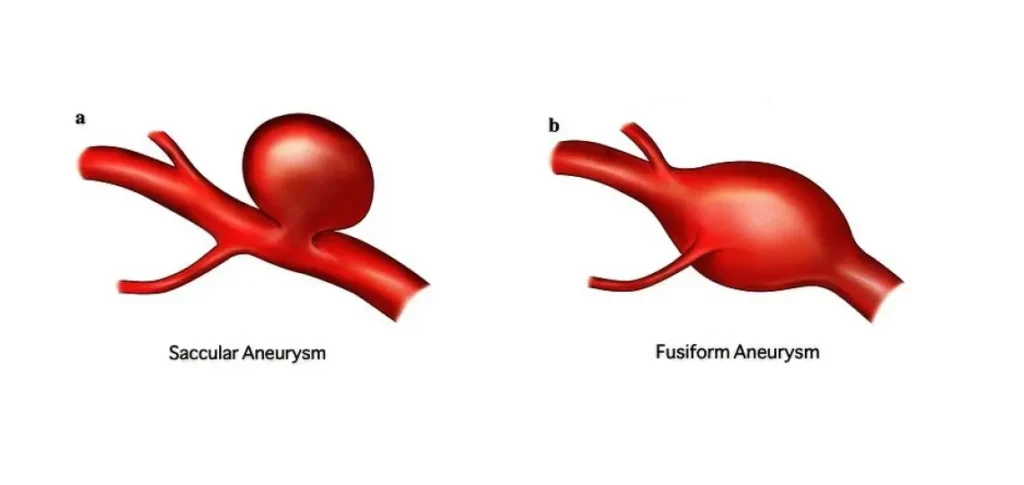
An arterial bulge or enlargement is called an aneurysm. Despite being silent, an aneurysm can cause major issues and occasionally even death. Any region of the body, including the brain and nervous system, can develop an aneurysm.
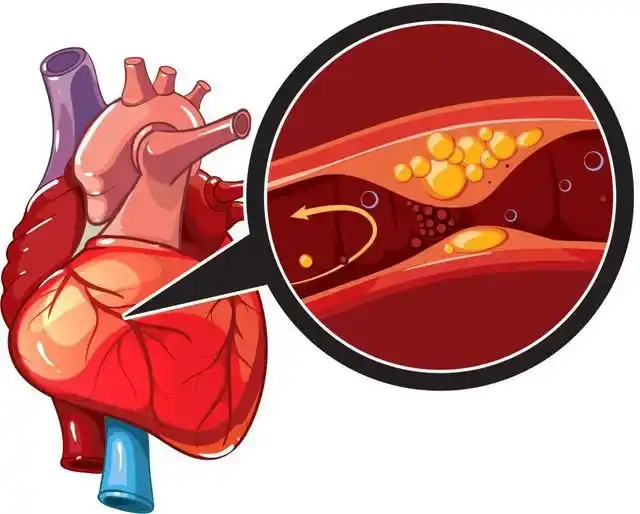
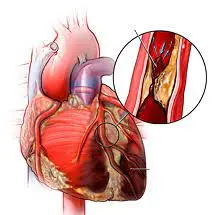
Atherosclerosis
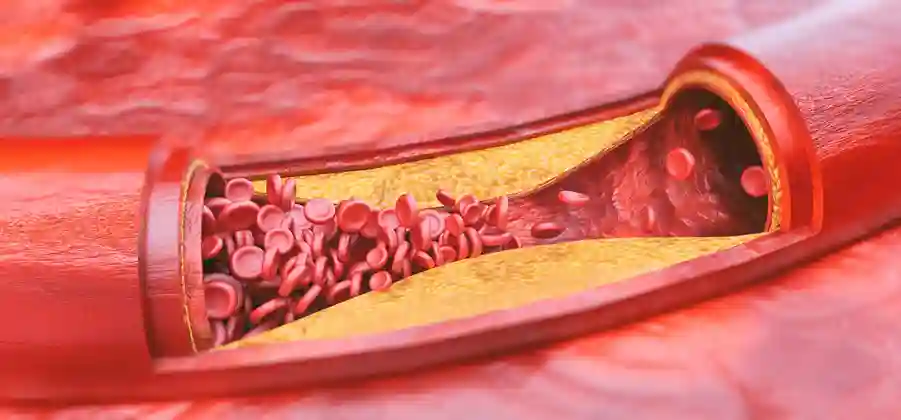
In this condition, fat deposits known as plaques build up and cause the artery walls to become thick and rigid. Consequently, the system’s blood flow is constrained. Every part of the body is susceptible to atherosclerosis. Coronary artery disease is the result of atherosclerosis in the heart. Peripheral artery disease is the cause if this happens in the legs.
Individuals with heart failure and hypertensive heart disease are more susceptible to:
- Decompensated cardiac failure.
- Acute coronary syndrome.
- Sudden cardiac death.
Signs and symptoms
The presence or absence of heart failure will determine the signs and symptoms of hypertensive heart disease. Hypertension, with or without left ventricular hypertrophy, is typically asymptomatic in the absence of heart failure.
Congestive heart failure symptoms, indicators, and outcomes can include:
- fatigue
- Palpitations or an irregular pulse
- Swelling in the ankles and feet
- Gaining weight
- nausea
- Breathlessness and trouble staying flat in bed (orthopnea)
- Abdominal pain and bloating
- More urgency to urinate at night
- Heart enlargement (cardiomegaly)
- Hypertrophy and remodeling of the left ventricle.
- Myocardial ischemia that is quiet and reduced coronary flow reserve
- Accelerated atherosclerosis and coronary heart disease
- Diastolic heart failure is another name for heart failure with normal left ventricular ejection fraction (HFNEF).
- Sudden cardiac death, atrial fibrillation, or other cardiac arrhythmias
Patients may appear with acute heart failure, acute decompensated heart failure, or pulmonary oedema as a result of an abrupt breakdown of the heart’s pump function. Heart failure can also develop gradually over time. Several factors, such as myocardial ischemia, significant elevations in blood pressure, or cardiac arrhythmias, can induce sudden failure.
Diagnosis and Tests
How is a diagnosis of hypertensive heart disease made?
Because high blood pressure doesn’t generate any symptoms, it’s important to visit your doctor often. Your provider will wish to acquire:
- Your medical background.
- your family’s history of heart disease.
- A physical exam.
Which tests are going to be performed to identify hypertensive heart disease?
Your doctor will seek to rule out ischemic cardiomyopathy and other conditions that might lead to heart failure. Tests consist of:
- Blood tests.
- Urine test.
- EKG stands for electrocardiogram.
- Echocardiogram for certain individuals.
Management
Which drugs are prescribed to treat hypertensive heart disease?
Although side effects are possible with any medication, it’s crucial to continue taking it. Your physician might be able to change your prescription if you’re concerned about a side effect. The following medications are used to treat high blood pressure:
- Diuretics force your body to eliminate extra fluid.
- Calcium channel blockers increase the opening of your blood vessels.
- Inhibitors of the angiotensin-converting enzyme that aid in blood vessel relaxation.
- Angiotensin II receptor blockers help in blood vessel relaxation.
- Vasodilators that facilitate the widening of blood arteries.
- Renin inhibitors that aid in blood vessel relaxation.
- Beta blockers lower your heart rate and facilitate the function of your heart.
Cerebrovascular Heart Disease
The disorder known as cerebrovascular heart disease affects the flow of blood to the brain. The primary cause of this is atherosclerosis. As was previously mentioned, atherosclerosis is a disorder where fat deposits build up and cause the walls of arteries to become thick and rigid.
Blood pressure can cause ischemic stroke by affecting blood flow, and an increase in blood pressure can cause blood vessels to tear, which can result in cerebral hemorrhage.
Causes
The basic or primary causes of cardiovascular heart disease are aneurysms, low-fat conditions, embolism, and atherosclerosis. Obesity, diabetes, smoking, and hypertension are risk factors.
Treatment
Cardiovascular disease is treated with medication, lifestyle modifications, and surgery.
Among the pharmaceuticals are blood thinners (heparin, warfarin), antiplatelets (aspirin, clopidogrel), and anti-diabetic drugs.
Among the surgeries are:
- Vascular surgery
- Endovascular operations
Inflammatory Heart Disease
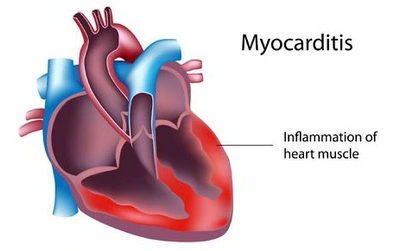
Your heart’s response to injury or infection is known as cardiac inflammation. Some may experience unexpected cardiac inflammation. It takes longer for others. While some people hardly have any symptoms, others have severe ones. Individual factors and causes can also affect how much inflammation a person has.
Your heart’s inflammation can be divided into three distinct regions.
Heart inflammation types
Endocarditis affects the valves that regulate blood flow from one chamber to another, as well as the lining of the heart chambers through which blood passes.
In myocarditis, the heart-pumping muscle is affected.
In pericarditis, the sac surrounding your heart is affected.
What is the cause of inflammation in the heart?
The majority of heart inflammation cases are caused by infections, typically by bacteria or viruses. Other reasons are as follows:
- Rheumatoid arthritis is one example of an autoimmune disease.
- Items in your surroundings, like lead.
- Medications, such as those for weight reduction, seizures, or depression.
- Following the COVID-19 vaccine, some young individuals have reported developing myocarditis or pericarditis. But after receiving medication, the majority made a full recovery.
How do you describe the symptoms?
All three forms of cardiac inflammation frequently present with the following symptoms:
- Chest pain.
- Breathlessness.
- Fever.
- Depending on the kind of inflammation in your heart, you may have additional symptoms.
Symptoms of endocarditis include:
- You have stomach pain.
- You have blood in your urine.
- Sweats during the night.
Symptoms of myocarditis include:
- Enlargement of your feet or legs.
- Heart palpitations.
- Excessive fatigue.
The following are signs of pericarditis:
- Rapid heartbeat.
- Pain in the chest that goes away as you sit up and bend forward.
If a virus is the cause of your heart inflammation, you may initially experience symptoms like:
- Runny nose.
- Cough.
- Stomach problems.
Diagnosis and Tests
How is inflammation of the heart diagnosed?
To determine whether you have heart inflammation, your doctor will look at the following:
- Physical examination.
- Your medical background.
- Tests, including blood tests.
What examinations will be performed to identify inflammation in the heart?
To assist them, your healthcare professional may do the following tests:
- Disqualify a heart attack.
- Examine the fluid surrounding your heart.
- Examine your heart’s functioning to determine whether it is abnormal.
Tests consist of:
- Computed tomography of the heart (CT).
- EKG stands for electrocardiogram.
- Echocardiogram.
- MRI of the heart.
- PET scan (positron emission tomography).
Management
How is inflammation of the heart treated?
Medication can help prevent infections and prevent your heart and immune system from overworking. You might require surgery or medical equipment if your issues are more severe.
Which drugs are taken?
Depending on the area of your heart that is inflamed, different medications may be used to treat it. Among the medications you may take are:
- Corticosteroids.
- Antibiotics.
- Antifungal medications.
- Medications that reduce inflammation.
- Medications for heart failure.
- Blood thinners.
Treatment side effects
The following side effects could occur, depending on the medication you’re taking:
- Diarrhea.
- Dizziness.
- Weakness.
- Pain in the abdomen.
Ischemic Heart Disease
Ischemia, also known as ischemic/ischemic heart disease, is a disorder where the heart’s blood flow is restricted, causing it to starve of oxygen.
This is most frequently caused by a buildup of plaque, which is a mixture of fatty material and cells, in the wall of the coronary arteries, which are one of the arteries that deliver blood to the heart. The plaque gradually blocks blood flow as it grows, depriving the heart of oxygen and nourishment.
Additionally, the plaque may rupture abruptly, tearing away from the arterial wall. This might result in a clot that forms quickly and blocks blood flow. The heart cells stop receiving blood, stop working, and eventually die as a result.
Types of ischemic heart disease
- Stable Angina
- Unstable Angina
- Myocardial Infarction (Heart Attack)
- Variant Angina (Prinzmetal’s Angina)
Ischemic Heart Disease Causes
Diabetes mellitus, high cholesterol, and smoking are risk factors.
- Hereditary and genetic factors may potentially contribute to this diseases.
- High blood pressure
- Another risk factor is stress.
What signs and symptoms are present in ischemic heart disease?
Among the most typical signs of ischemic heart disease are:
- Angina, or chest pain
- Fatigue,
- sweating,
- Palpitations, and
- Shortness of breath
Medical Intervention
Medications used to treat ischemic heart disease include
- Non-specific smooth muscles can be relaxed with the use of organic nitrates.
- Beta-blockers enhance oxygen consumption and decrease heart work.
- Angina risk is decreased with aspirin.
- By inhibiting beta receptors, calcium channel blockers lower total coronary flow.
Risk Factors for Heart Disease
Your risk of heart disease might be raised by several things. Certain populations and people with specific underlying conditions are at higher risk of acquiring heart disease.
Non-Modifiable
Among the risk factors that cannot be changed are:
- Age
- Early heart disease in the family history
- Genetics
Modifiable
Among the modifiable risk factors are:
- Smoking or being around secondhand smoke regularly
- Absence of physical activity and exercise
- Sleep disorders such as insomnia or inadequate or irregular sleep
- Anxiety
- unhealthy diet, particularly one that has a lot of processed carbs and saturated fats
- Environmental factors (such as pollution and working conditions)
Underlying Conditions
Additionally, having any of the following diseases or disorders increases your risk of developing heart disease:
- Hypertension, or elevated blood pressure,
- elevated levels of the “bad” cholesterol known as low-density lipoprotein (LDL)
- Elevated blood triglyceride levels
- Atherosclerosis
- Psoriasis, ulcerative colitis, Crohn’s disease, and other autoimmune inflammatory diseases
- Diabetes mellitus
- Chronic kidney disease
- Obesity or being overweight
- HIV stands for human immunodeficiency virus.
- Anxiety, depression, or other mental health issues
- The metabolic syndrome is a collection of symptoms that, when present, increase the risk of heart disease, stroke, and type 2 diabetes.
Preventing Heart Disease
There are things you can do to lower your risk and avoid heart disease. The majority entail altering lifestyle choices, including the following, to enhance general health:
- Consume a heart-healthy diet that includes a variety of fruits and vegetables, foods low in trans and saturated fats, added sugar, and salt, and alcohol in moderation.
- Engage in regular exercise: Try to get 150 minutes a week of light to moderate exercise, such as swimming, cycling, walking, or jogging.
- Give up smoking: Smoking raises your risk of developing heart disease. If you smoke, discuss your quitting alternatives with your healthcare physician.
- Keep your weight under control since too much weight might strain your heart and blood vessels.
- Get adequate sleep: Aim for seven to eight hours per night. You can enhance the quality of your sleep by adhering to a sleep routine.
- Track the risk factors: Control any underlying health issues that increase your risk by using prescription drugs or altering your lifestyle to control high blood pressure, diabetes, and other risk factors.
Heart Disease Treatment
Depending on the type of heart disease you have, treatment options may include medication, surgery, or lifestyle modifications.
Lifestyle changes
One important part of traditional treatment for CVD is prevention, which can include:
- Making dietary changes
- Increasing physical activity levels or adding exercise
- Giving up smoking
- Make sure you’re sleeping well
- Stress-reduction methods, including yoga, mindfulness, and others
Drugs
The goal of heart disease prescription drugs is to manage risk factors to avoid problems or lessen symptoms. For CVD, several classes are taken into consideration.
- Drugs called angiotensin-converting enzyme (ACE) inhibitors are used to treat heart failure and excessive blood pressure. Lotensin (benazepril) and captopril are two examples.
- Beta-blockers, such as Tenormin (atenolol) and Lopressor (metoprolol), reduce blood pressure, treat cardiac arrhythmias, and stop a second heart attack.
- Antidiabetics, such as Jardiance (empagliflozin), Invokana (canagliflozin), and Victoza (liraglutide), are medications used to lower blood sugar levels in diabetics. They also lower the chance of complications if you have heart disease and diabetes.
- In order to treat CVD and restore blood flow, nitrates, such Nitrostat (nitroglycerin), dilate blood arteries.
- Mevacor (lovastatin) and Livalo (pitavastatin) are two examples of statins that lower cholesterol and lower the risk of heart disease. If you have diabetes or are at increased risk, your doctor might suggest a statin.
Alternative & Complementary Medicine
Alongside conventional treatments, some heart disease patients employ a variety of complementary and alternative medicine (CAM) techniques. These consist of:
Certain supplements
- Yoga
- Tai chi and meditation
- Consult a healthcare professional before putting these strategies into practice.
Percutaneous Coronary Intervention
Healthcare professionals can treat CVD by treating blockages or obstructions in the arteries with a minimally invasive procedure called percutaneous coronary intervention (PCI), often known as angioplasty with stent implantation. To stop the artery from shutting, a stent—a mesh support tube—is inserted following the procedure.
Coronary Artery Bypass Grafts
In bypass surgery, also known as coronary artery bypass graft (CABG), a surgeon reroutes the heart’s blood supply by using healthy veins from the chest wall. The obstruction is circumvented by the recently connected vessels. Usually, this treatment is saved for more serious or involved patients.
Myocardial Revascularization.
Myocardial revascularization is a procedure used by medical professionals to repair heart blockages and blood clots when previous operations for CVD are not successful or advised. To make it easier for blood to flow from the left ventricle to the center of the heart, these treatments use lasers to make holes in the heart’s walls.
Living with heart disease.
Since heart disease necessitates lifestyle modifications as well as adherence to prescriptions and checkups, managing it can be difficult. It’s critical to understand how to manage your disease and where to look for support. Here are some pointers:
- Speak with your provider: Get advice from your provider if you need to change your diet, increase exercise, or require more assistance. They might be able to direct you to beneficial experts, initiatives, and materials.
- Ask for help from friends and family: Don’t be scared to ask for help from your friends and family; talk to them about what you’re going through.
- Consider therapy. You can learn stress management techniques and cope with your diseases by attending individual or group sessions with a mental health expert.
- Keep a health log: During checkups, it can be useful to have a record of your prescriptions and any odd symptoms.
- Look for assistance online: Support groups for people with heart disease are also available. Message boards and social media pages can be extremely important information and community resources.
- Advocacy groups: Heart research is promoted by advocacy groups like the American Heart Association.
Heart Disease Prognosis
Being proactive in controlling heart disease is essential since complications, such as heart attacks, become significantly more dangerous the second or third time they happen. According to a comprehensive assessment, almost half of the patients who were readmitted to the hospital for a second heart attack within ninety days of the first passed away within five years.
However, you can lower your risk of future cardiac events or consequences by controlling risk factors, adopting healthy lifestyle practices, and taking your medicine as directed.
FAQs
What is heart disease?
Heart disease encompasses a range of conditions that can impact your heart. People frequently think about coronary artery disease (CAD), the most prevalent kind of heart disease, and the heart attacks it can cause. However, you might experience issues with your heart’s electrical system, valves, or cardiac muscle.
What is the term for heart disease in medicine?
Cardiovascular disease is the medical term for heart disease. What kinds of heart diseases are there? Rheumatic fever is the cause of rheumatic heart disease, a persistent heart disorder. This heart condition is extremely prevalent in kids. This diseases is more common in emerging nations, particularly in impoverished communities.
What leads to heart disease?
Heart disease has been associated with diets heavy in fat, salt, sugar, and cholesterol. High blood pressure. Uncontrolled high blood pressure can lead to thickening and hardening of the arteries. These modifications affect how blood flows to the body and heart. high cholesterol. The risk of atherosclerosis is increased by elevated cholesterol.
What physical effects does heart disease have?
Several components of your heart and circulatory system, including the arteries that transport blood to and from the heart and the valves that open and close to maintain blood flow in the proper direction at the appropriate time, can be impacted by heart disease. (Image Source: Getty Images/iStock) The leading cause of death and the most prevalent cardiac condition is CAD.
Is there only one type of heart disease?
There are several types of heart disease. Several problems might impact the function of your heart. Cardiovascular disease is another name for heart disease, and it also refers to issues with blood arteries. About 1 in 5 deaths, or 700,000 deaths annually, in the United States are attributable to heart disease.
Is a normal life possible for someone with heart disease?
Even though congestive heart failure restricts an adult’s activities, many people can still enjoy life with the correct care and treatment plan. Taking your prescription drugs is one way to take care of yourself.
What is the onset age of heart problems?
According to data from the American Heart Association, the average age of a person in the United States at the time of their first heart attack is 72 years for women and 65.5 years for men. But those figures are shifting. According to a 2019 ACC publication, heart attacks are becoming more common in people under 40.
How can I tell whether my heart is healthy?
You can use these methods to determine whether your heart is healthy today and in the future.
heart rate. Between 60 and 100 beats per minute is the typical resting heart rate for most adults.
The ability to breathe, blood pressure, energy levels, oral health, etc.
Attend all of your screenings.
Reference
- Heart. (2023, November 3). Kenhub. https://www.kenhub.com/en/library/anatomy/heart
- Rheumatic heart disease. (2025, February 13). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21485-rheumatic-heart-disease
- Valvular heart disease: causes, symptoms and treatment. (n.d.). Best Hospitals in India | Medicover Hospitals. https://www.medicoverhospitals.in/diseases/heart-valve-diseases/
- Hypertensive heart disease. (2024, May 1). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/21840-hypertensive-heart-disease
- Heart inflammation. (2025, January 2). Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/23052-heart-inflammation
- Victor Chang Cardiac Research Institute. (n.d.). Ischaemic heart disease: symptoms, causes & treatment – Victor Chang Cardiac Research Institute. The Victor Chang Cardiac Research Institute. https://www.victorchang.edu.au/heart-disease/ischaemic-heart-disease
- Gurarie, M. (2023, May 12). What is heart disease? Verywell Health. https://www.verywellhealth.com/heart-disease-7481236
- World Health Organization: WHO. (2021, June 11). Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)



23 Comments