Type 1 Diabetes
What is Type 1 Diabetes?
Type 1 diabetes, often referred to as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition in which the pancreas produces little to no insulin. Insulin is a vital hormone responsible for regulating blood sugar levels, enabling the body to convert glucose into energy.
Insulin is a vital hormone that regulates blood glucose (sugar) levels. Insulin works in the following ways under normal conditions:
After breaking down the food you eat, your body uses glucose, or sugar, as its primary energy source.
As soon as glucose enters your bloodstream, your pancreas releases insulin.
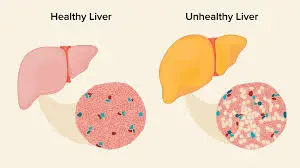
Insulin facilitates the uptake of blood glucose by muscle, fat, and liver cells, allowing them to either use it as fuel or store it for later use.
It tells your pancreas to cease making insulin when glucose enters your cells and blood glucose levels drop.
When you don’t have enough insulin, your body can’t use the food you eat for energy because too much sugar accumulates in your blood, known as hyperglycemia. If left untreated, this might result in severe health issues or even death. To survive and maintain their health, people with Type 1 diabetes require synthetic insulin daily.
Insulin-dependent diabetes and juvenile diabetes were earlier names for type 1 diabetes.
Type 1 diabetes vs. type 2 diabetes?
Although both Type 1 and Type 2 diabetes cause hyperglycemia, or elevated blood sugar, they are different types of diabetes mellitus (as opposed to diabetes insipidus).
Insulin resistance is typically the cause of Type 2 diabetes (T2D), characterized by insufficient insulin production by the pancreas and/or inefficient insulin use by the body. Type 2 diabetes can be brought on by a combination of hereditary and lifestyle factors, such as weight and inactivity.
In individuals with Type 1 diabetes, the pancreas does not make insulin. An autoimmune reaction is the cause.
Type 2 diabetes usually affects older people, while it is becoming more common in youth. Type 2 diabetes usually affects older people, while it is becoming more common in youth. Although type 1 diabetes can strike anyone at any age, it typically strikes children or young adults.
Who is affected by Type 1 diabetes?
Although Type 1 diabetes (T1D) can strike anyone at any age, it is most frequently diagnosed in early adolescence (10–14 years old) and between the ages of 4 and 6.
Type 1 diabetes affects persons assigned female at birth almost equally to those designated male, and it is most common among non-Hispanic white people in the United States.
Although having a parent or sibling with Type 1 diabetes raises your risk of getting the disease, you do not need to have a family member with the disease to have it.
How common is Type 1 diabetes?
Diabetes type 1 is rather prevalent. About 1.24 million Americans currently have Type 1 diabetes, and by 2050, that figure is predicted to rise to five million.
Although it can also strike adults, type 1 diabetes is one of the most prevalent chronic illnesses affecting children in the US.
Symptoms and Causes:
What signs of Type 1 diabetes are present?
Type 1 diabetes symptoms usually begin mildly and gradually worsen or intensify for a few days, weeks, or months. This occurs as a result of your pancreas releasing less and less insulin.
Symptoms of Type 1 diabetes include:
- Excessive thirst.
- frequent urine, including bedwetting in children and frequent full diapers in babies.
- Excessive appetite.
- Inexplicable loss of weight.
- Fatigue.
- visual impairment.
- Cuts and sores heal slowly.
- yeast infections in the vagina.
- It’s critical to visit your doctor and get a Type 1 diabetes test as soon as possible if you or your child exhibit these symptoms. Getting a diagnosis as soon as feasible is ideal.
Diabetes-related ketoacidosis (DKA), a consequence of uncontrolled Type 1 diabetes, can be fatal if a diagnosis is postponed. If any of the following symptoms apply to you or your child, get emergency medical attention:
- breath with a fruity scent.
- vomiting and nausea.
- Abdominal Pain
- breathing quickly.
- Confusion.
- Drowsiness.
- unconsciousness.
What causes Type 1 diabetes?
When your immune system unintentionally targets and kills the insulin-producing cells in your pancreas, type 1 diabetes results. For months or years, this degradation may occur, leading to an absolute lack of insulin (deficiency).
Although the precise origin of Type 1 diabetes is still unknown, scientists think there is a significant genetic component. Without a family history, the chance of getting the illness is about 0.4%. You have a 30% chance of getting Type 1 diabetes if both of your biological parents have the disease.
Scientists believe that if you are genetically predisposed to Type 1 diabetes, your immune system may target pancreatic cells due to environmental toxins or viruses.
Diagnosis and Tests:
How is Type 1 diabetes diagnosed?
Diagnosing type 1 diabetes is quite easy. Your doctor will request the following tests if you or your kid exhibit signs of Type 1 diabetes:
Blood glucose test: Your healthcare provider does a blood glucose test to determine how much sugar is in your blood. They might ask you to do a fasting test (no food or liquids for at least eight hours before the test) and a random test (no fasting). You usually have Type 1 diabetes if the results indicate that your blood sugar is high.
Glycosylated hemoglobin test (A1c): Your healthcare provider may do an A1c test if the results of a blood glucose test show that you have diabetes. Your average blood sugar levels over the last three months are determined by this.
Antibody test: This blood test determines if you have Type 1 or Type 2 diabetes by looking for autoantibodies. Proteins called autoantibodies unintentionally target the tissue in your body. Type 1 diabetes is indicated by specific autoantibodies.
To evaluate your general health and determine whether you have diabetes-related ketoacidosis, a dangerous acute consequence of undiagnosed or untreated Type 1 diabetes, your doctor will also probably conduct the following tests:
Basic metabolic panel: This test uses a blood sample to measure eight distinct chemicals in your blood. The panel offers useful details on the metabolism and chemical balance of your body.
Urinalysis: A urinalysis, sometimes referred to as a urine test, is a test that looks at the microscopic, chemical, and visual components of your urine. Providers utilize it to measure certain parameters connected to urine. If a Type 1 diagnosis is made, the test will probably be ordered to look for ketones, a chemical your body makes when it must use fat as fuel rather than glucose. Your blood becomes acidic when you have too many ketones, which can be fatal.
Arterial blood gas: An arterial blood gas (ABG) test takes a sample from an artery in your body to determine the levels of oxygen and carbon dioxide in your blood.
Management and Treatment:
What kind of doctor treats Type 1 diabetes?
People with Type 1 diabetes are treated by endocrinologists, medical professionals who specialize in treating disorders connected to hormones. Diabetes is a specialty of several endocrinologists.
Your child needs to see a pediatric endocrinologist if they have Type 1 diabetes.
To make sure that your Type 1 diabetes treatment is going well, you will need to see your endocrinologist on a frequent basis. As you age, your insulin requirements will also alter.
How is Type 1 diabetes treated?
To survive and maintain their health, people with Type 1 diabetes require synthetic insulin daily, sometimes times a day. Additionally, they must make an effort to maintain a healthy range for their blood sugar.
The therapy for Type 1 diabetes is complicated and very customized because some factors influence your blood sugar level.
Three key elements of managing Type 1 diabetes are as follows:
- Insulin.
- Blood glucose (sugar) monitoring.
- Carbohydrate counting.
Insulin as a Type 1 diabetes treatment:
Synthetic insulin comes in some varieties. They all begin to function at varying rates and remain in your body for varying amounts of time. It could be necessary to employ many types.
Inulin comes in a variety of price points. To determine which kind of insulin is best for you, consult your endocrinologist.
Your daily insulin requirements are determined by some factors, including:
- Your weight.
- Your age.
- Your physical activity level.
- The types of food you eat.
- Your current blood sugar (glucose) level.
- You must give yourself certain amounts of insulin when you eat and treat elevated blood sugar levels, in addition to your baseline level of insulin (commonly referred to as a basal rate).
The following methods can be used to consume insulin:
Multiple daily injections (MDI): A vial and syringe are used to administer injectable insulin. Using a syringe, you extract the appropriate amount of insulin from the vial for each injection. It is possible to inject insulin into the fat in your abdomen, upper arms, thighs, or buttocks. Insulin injections are typically the least expensive method of administration.
Pen: Insulin is pre-filled in insulin pens, which resemble injections. Generally speaking, disposable pen needles are more practical than syringes. For those with low eyesight, they may also be a viable choice.
Pump: Insulin pumps are machines that continuously and sporadically deliver insulin. They mimic the way your pancreas naturally releases insulin. Pumps deliver insulin by a tiny catheter, a thin, flexible tube, which is placed into your abdomen or another fleshy area of your body.
Rapid-acting inhaled insulin: Like an asthma inhaler, this kind of insulin is inhaled through the lips. Compared to other forms of insulin, it acts considerably more quickly.
Throughout your life and in different situations, your daily insulin requirements will change. For instance, throughout puberty, and pregnancy, and while taking steroid treatment, you usually require higher amounts of insulin.
To ensure that your insulin dosages and general diabetes care are working for you, you must see an endocrinologist regularly, usually at least three times a year.
Monitoring blood sugar levels to control Type 1 diabetes:
Individuals with Type 1 diabetes must constantly check their blood sugar levels. The best defense against health issues is to keep blood sugar levels within a safe range. The following methods can be used to keep an eye on your blood sugar:
Blood glucose meter: A tiny drop of blood is placed on the test strip of the meter after you prick your finger. The meter displays your blood glucose level in a matter of seconds. A blood glucose meter is usually the least expensive option for at-home testing, even if it only shows your blood sugar at the time of the test.
Continuous glucose monitoring (CGM): Different kinds of CGMs exist. Every seven to fourteen days, you must place a tiny sensor beneath your skin at home to use the majority of CGMs. A medical professional may implant certain CGMs. Your blood glucose levels are continuously recorded by the sensor. Finger sticks are less necessary for those who use a CGM. Compared to fingerstick blood glucose meters, CGM systems can be more costly, but they offer a lot more information about your blood sugar levels, including their history and future directions. To notify you if your blood sugar is trending too high or too low, you can set up various alarms.
Your target blood glucose level range will be determined by your healthcare practitioner. Numerous variables influence it, such as your:
- Age.
- Lifestyle.
- Overall health.
- Access to diabetes technology and supplies.
Counting carbohydrates to control Type 1 diabetes:
Counting the number of carbohydrates in the foods and beverages you eat and drink is a big component of managing Type 1 diabetes because it helps you get the right amount of insulin.
Some foods and beverages, including grains, sweets, legumes, and milk, include carbohydrates, a type of macronutrient. Glucose, the primary energy source for the body, is created when carbs in food and drink are broken down.
As a result, upon consuming carbs, persons with Type 1 diabetes must administer insulin to themselves.
At its most basic, carb counting is calculating how many grams of carbohydrates are in a meal (by looking at nutrition labels) and comparing that to your insulin dosage.
To determine how much insulin you need to take to control your blood sugar levels while eating, you’ll utilize a ratio called insulin-to-carbs. Each person has a different insulin-to-carb ratio, which may even change during the day. You can find out your insulin-to-carb ratio with the assistance of an endocrinologist.
What are the side effects of diabetes treatment?
Hypoglycemia, or low blood sugar, is the primary adverse consequence of insulin-assisted diabetic treatment. Depending on your food intake and/or degree of activity, taking too much insulin can result in low blood sugar. Generally speaking, hypoglycemia is defined as less than 70 mg/dL (milligrams per deciliter).
Low blood sugar symptoms can appear suddenly, and each person will experience them differently. Although hypoglycemia symptoms are unpleasant, they serve as helpful indicators that you should act before your blood sugar levels continue to fall.
The symptoms of low blood sugar include:
- Shaking or trembling.
- Sweating and chills.
- Dizziness or lightheadedness.
- Faster heart rate.
- Headaches.
- Hunger.
- Nausea.
- Nervousness or irritability.
- Pale skin.
- Restless sleep.
- Weakness.
- Hypoglycemia must be treated immediately because it can be harmful.
The “15-15 rule,” as advised by the American Diabetes Association, for a low blood sugar episode entails:
- Consuming 15 grams of carbohydrates through food or drink increases blood sugar levels.
- Verify your blood sugar levels after fifteen minutes.
- If it remains below 70 mg/dL, consume an extra 15 grams of carbs.
- Until you feel better, follow the 15-15 rule if you experience hypoglycemia symptoms but are unable to check your blood sugar.
To treat lows, children usually require fewer grams of carbohydrates. Consult their physician.
Does Type 1 diabetes have a treatment?
Although there isn’t a treatment for Type 1 diabetes at this time, researchers are using TrialNet and other trials to try to prevent or halt the disease’s progression.
Additionally, researchers are investigating pancreatic islet transplantation, an experimental treatment for brittle diabetes.
Clusters of cells in the pancreas called pancreatic islets are responsible for producing insulin. When you have Type 1 diabetes, your immune system targets these cells. With a pancreatic islet transplant, damaged islets are swapped out with new ones that produce and secrete insulin. Through this process, islets from an organ donor’s pancreas are transferred to a patient who has Type 1 diabetes. Only those who are engaged in a study can undergo pancreatic islet transplantation because the process is still being studied.
Is Type 1 diabetes preventable?
Regretfully, there is nothing you can do to avoid becoming Type 1.
Your doctor may test members of your family for the autoantibodies that cause Type 1 diabetes because the condition can run in families. Autoantibody testing is also available to family members of individuals with Type 1 diabetes through the international research network Type 1 Diabetes TrialNet.
Even in the absence of diabetes symptoms, having autoantibodies increases your risk of Type 1 diabetes. You might want to get an autoantibody test if you have a parent, sibling, or child with Type 1 diabetes. Early detection of Type 1 diabetes can be aided by these tests.
Summary:
The chronic disease known as type 1 diabetes occurs when the immune system of the body unintentionally targets and kills the insulin-producing cells in the pancreas. Insulin is a hormone that helps regulate 1 blood sugar levels. Without insulin, sugar cannot enter the body’s cells for energy, leading to a buildup of sugar in the bloodstream.
FAQ:
Is it possible to cure type 1 diabetes?
Type 1 diabetes currently has no known cure. But our understanding of the illness is always changing. Researchers are making significant advances and developing new technologies and medications. At any age, people with type 1 diabetes are currently leading active, healthy lives.
What makes type 1 diabetes different from type 2 diabetes?
In individuals with type 1 diabetes, the pancreas is unable to produce insulin because the immune system attacks the islet cells that make the hormone. Insulin resistance develops in people with type 2 diabetes, and the pancreas produces less insulin than it once did.
Is a long life possible for someone with type 1 diabetes?
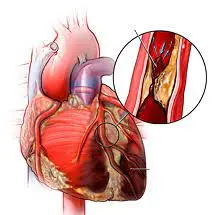
People with type 1 diabetes continue to die young, mostly from cardiovascular disease (CVD), even though their longevity has gradually extended since the introduction of insulin therapy. A subset of people with type 1 diabetes, however, live long lives with little to no morbidity.
What causes type 1 diabetes?
It is believed that an autoimmune reaction—in which the body unintentionally targets itself—causes type 1 diabetes. The beta cells in the pancreas, which produce insulin, are destroyed by this process. Before any symptoms show up, this process may continue for months or even years.
Can people with type 1 diabetes consume sugar?
You don’t have to cut out sugar from your diet if you have diabetes. Sugar doesn’t directly cause type 1 diabetes because the exact origin of the disease is unknown and unrelated to lifestyle choices. There is some complexity surrounding the subject of whether sugar directly causes type 2 diabetes.
Is type 1 diabetes self-correcting?
Diabetes cannot be completely cured or eliminated. Most people can reverse their diabetes, though. In order to reverse diabetes, blood sugar levels must be continuously monitored until medication is no longer needed. A healthy diet and regular exercise are then necessary to maintain that control level.